Total Hip Replacement

If your hip has been damaged by arthritis, a fracture or other conditions,common activities such as walking or getting in and out of a chair may be painful and difficult. Your hip may be stiff and it may be hard to put on your shoes and socks. You may even feel uncomfortable while resting.
If medications, changes in your everyday activities, and the use of walking aids such as a cane are not helpful, you may want to consider hip replacement surgery. By replacing your diseased hip joint with an artificial joint, hip replacement surgery can relieve your pain, increase motion, and help you get back to enjoying normal, everyday activities.
First performed in 1960, hip replacement surgery is one of the most important surgical advances of the last century. Since 1960, improvements in joint replacement surgical techniques and technology have greatly increased the effectiveness of total hip replacement.
Anatomy
The hip is one of the body's largest weight-bearing joints. It consists of two main parts: a ball (femoral head) at the top of your thighbone (femur) that fits into a rounded socket (acetabulum) in your pelvis. Bands of tissue called ligaments (hip capsule) connect the ball to the socket and provide stability to the joint.
The bone surfaces of the ball and socket have a smooth durable cover of articular cartilage that cushions the ends of the bones and enables them to move easily.
A thin, smooth tissue called synovial membrane covers all remaining surfaces of the hip joint. In a healthy hip, this membrane makes a small amount of fluid that lubricates and almost eliminates friction in your hip joint.
Normally, all of these parts of your hip work in harmony, allowing you to move easily and without pain.
Common Causes of Hip Pain and Loss of Hip Mobility
The most common cause of chronic hip pain and disability is arthritis. Osteoarthritis, rheumatoid arthritis, and traumatic arthritis are the most common forms of this disease.
- Osteoarthritis usually occurs in people 50 years of age and older and often individuals with a family history of arthritis. It may be caused or accelerated by subtle irregularities in how the hip developed. In this form of the disease, the articular cartilage cushioning the bones of the hip wears away. The bones then rub against each other, causing hip pain and stiffness.
- Rheumatoid arthritis is an autoimmune disease in which the synovial membrane becomes inflamed, produces too much synovial fluid, and damages the articular cartilage, leading to pain and stiffness.
- Traumatic arthritis can follow a serious hip injury or fracture. A hip fracture can cause a condition known as osteonecrosis. The articular cartilage becomes damaged and, over time, causes hip pain and stiffness.
Is Hip Replacement Surgery for You?
Whether to have hip replacement surgery should be a cooperative decision made by you, your family, your primary care doctor, and the orthopaedic surgeon. The process of making this decision typically begins with a referral to us for an initial evaluation.
Although many patients who undergo hip replacement surgery are 60 to 80 years of age, we evaluate patients individually. Recommendations for surgery are based on the extent of your pain, disability, and general health status-not solely on age.
You may benefit from hip replacement surgery if:
- Hip pain limits your everyday activities such as walking or bending.
- Hip pain continues while resting, either day or night.
- Stiffness in a hip limits your ability to move or lift your leg.
- You have little pain relief from anti-inflammatory drugs or glucosamine sulfate.
- You have harmful or unpleasant side effects from your hip medications.
- Other treatments such as physical therapy or the use of a gait aid such as a cane do not relieve hip pain.
The Orthopaedic Evaluation

We will review the results of your evaluation with you and discuss whether hip replacement surgery is the best method to relieve your pain and improve your mobility. Other treatment options such as medications, physical therapy, or other types of surgery also may be considered . The orthopaedic evaluation will typically include:
- A medical history, in which we gather information about your general health and ask questions about the extent of your hip pain and how it affects your ability to perform every day activities.
- A physical examination to assess hip mobility, strength, and alignment.
- X-rays (radiographs) to determine the extent of damage or deformity in your hip.
- Occasionally, blood tests or other tests such as MRI (magnetic resonance imaging or bone scanning may be needed to determine the condition of the bone and soft tissues of your hip.
What to Expect From Hip Replacement Surgery
An important factor in deciding whether to have hip replacement surgery is understanding what the procedure can and cannot do.
Most people who undergo hip replacement surgery experience a dramatic reduction of hip pain and a significant improvement in their ability to perform the common activities of daily living. However, hip replacement surgery will not enable you to do more than you could before your hip problem developed.
Following surgery, you will be advised to avoid certain activities, including jogging and high-impact sports, for the rest of your life. You may be asked to avoid specific positions of the joint that could lead to dislocation.
Even with normal use and activities, an artificial joint (prosthesis) develops some wear over time. If you participate in high-impact activities or are overweight, this wear may accelerate and cause the prosthesis to loosen and become painful.
Preparing for Surgery
Medical Evaluation
If you decide to have hip replacement surgery, you will be asked to have a complete medical examination before your surgical procedure. This is needed to assess your health and identify conditions that can interfere with your surgery or recovery.
Tests
Several tests may be needed to help plan your surgery: blood and urine samples may be tested and a cardiogram and chest x-rays (radiographs) may be obtained.
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact us for a program to improve your skin before surgery.
Blood Donations
You will need to arrange for blood donors. Blood arranged will be stored as you will need blood after surgery.
Medications
Tell us about the medications you are taking. We will advise you which medications you should stop or can continue taking before surgery.
Weight Loss
If you are overweight, you may be asked to lose some weight before surgery to minimize the stress on your new hip and possibly decrease the risks of surgery
Dental Evaluation
Although infections after hip replacement are not common, an infection can occur if bacteria enter your bloodstream. Because bacteria can enter the bloodstream during dental procedures, you should consider getting treatment for significant dental diseases (including tooth extractions and periodontal work) before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Urinary Evaluation
Individuals with a history of recent or frequent urinary infections and older men with prostate disease should consider a urological evaluation before surgery.
Social Planning
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry. You may have to make arrangements for home help and for personal needs at your home .
Home Planning
The following is a list of home modifications that will make your return home easier during your recovery:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new hip
- A reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
Your Surgery
You will most likely be admitted to the hospital a day prior to your surgery. Prior to admission, a member of the anesthesia team will evaluate you. The most common types of anesthesia for hip replacement surgery are general anesthesia (which puts you to sleep throughout the procedure and uses a machine to help you breath) or spinal epidural anesthesia (which allows you to breath on your own but anesthetizes your body from the waist down). The anesthesia team will discuss these choices with you and help you decide which type of anesthesia is best for you.
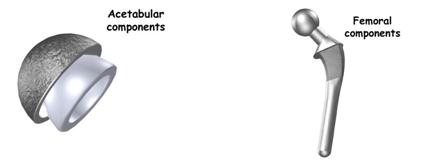
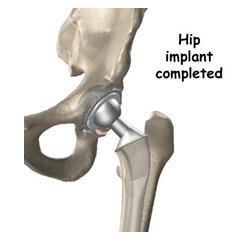
Many different types of designs and materials are currently used in artificial hip joints. All of them consist of two basic components: the ball component (made of a highly polished strong metal or ceramic material) and the socket component (a durable cup made of plastic, ceramic or metal, which may have an outer metal shell).
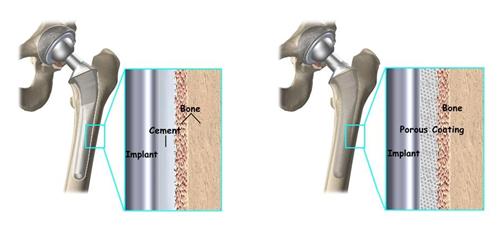
Special surgical cement may be used to fill the gap between the prosthesis and remaining natural bone to secure the artificial joint.
A non cemented prosthesis has also been developed and is used most often in younger, more active patients with strong bone. The prosthesis may be coated with textured metal or a special bone-like substance, which allows bone to grow into the prosthesis.
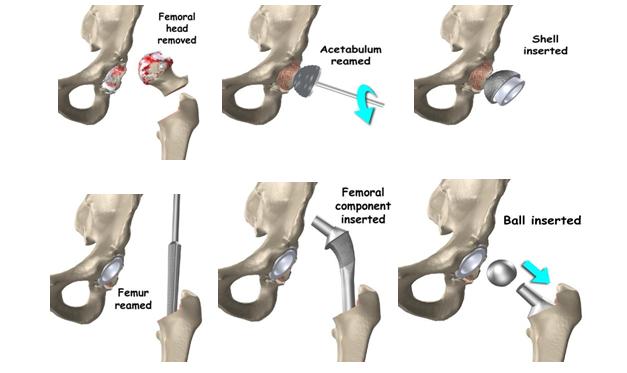
The surgical procedure involves removing the damaged cartilage and bone and then position new metal, plastic, or ceramic joint surfaces to restore the alignment and function of your hip.
Hybrid Total Hip Replacement
A hybrid total hip replacement has one component, usually the acetabular socket, inserted without cement, and the other component, usually the femoral stem, inserted with cement. This technique was introduced in the early 1980s . A hybrid hip takes advantage of the excellent track records of cementless hip sockets and cemented stems.
Partial Hip Replacements
If only one part of the joint is damaged or diseased, a partial hip replacement may be recommended. In most instances, the acetabulum is left intact and the head of the femur is replaced, using components similar to those used in a total hip replacement. The most common form of partial hip replacement is called a bipolar prosthesis.

Hip Resurfacing
A newer technique for hip replacement that has recently emerged is called hip resurfacing. In this procedure, the socket is replaced similar to a total hip replacement. The femur, however, is covered or "resurfaced" with a hemispherical component. This fits over the head of the femur and spares the bone of the femoral head and the femoral neck. It is fixed to the femur with cement around the femoral head and has a short stem that passes into the femoral neck.

Hip resurfacing is an emerging procedure, most commonly performed in younger patients.T he most important reason to do a hip resurfacing rather than a traditional artificial hip replacement, is to remove as little bone around the hip as possible. This is especially important when you may need a second, or revision, hip replacement as you grow older .
After surgery, you will be moved to the recovery room where you will remain for 1 to 2 hours while your recovery from anesthesia is monitored. After you awaken fully, you will be taken to your hospital room.
Minimally Invasive Total Hip Replacement
Over the past several years, we have developed new minimally invasive surgical techniques for inserting total hip replacement implants through smaller incisions.
This allows for quicker, less painful recovery and more rapid return to normal activities. Minimally invasive and small incision total hip replacement surgery is a rapidly evolving area. Although certain techniques have proven to be safe, others may be associated with an increased risk of complications, such as nerve and artery injuries, wound healing problems, infection, fracture of the femur, and malposition of the implants, which can contribute to premature wear, dislocation, and loosening of your hip replacement.
Patients who have marked deformity of the joint, those who are heavy or muscular, and those who have other health problems that can contribute to wound healing problems are not candidates for this technique .
Your Stay in the Hospital

You will usually stay in the hospital for 3-5 days. After surgery, you will feel pain in your hip. Pain medication will be given to make you as comfortable as possible.
To avoid lung congestion after surgery, you will be asked to breathe deeply and cough frequently.
To protect your hip during early recovery, a positioning splint, such as a V-shaped pillow placed between your legs, may be used.
Walking and light activity are important to your recovery and will begin the day of or the day after your surgery. Most patients who undergo total hip replacement begin standing and walking with the help of a walking support and a physical therapist the day after surgery. The physical therapist will teach you specific exercises to strengthen your hip and restore movement for walking and other normal daily activities.
Complications
The complication rate following Hip replacement surgery is low. Serious complications, such as joint infection, occur in fewer than 1% of patients. Major medical complications, such as heart attack or stroke, occur even less frequently.
Blood clots in the leg veins or pelvis are the most common complication of hip replacement surgery. For this you are made to start ankle pump exercises , put pressure stockings & take blood thinners .
Other complications such as dislocation, nerve and blood vessel injury, bleeding, fracture, and stiffness are very rare .
Over years, the hip prosthesis may wear out or loosen. This problem is less common with our newer materials and techniques. An average Total hip replacement lasts for 20 years .
Recovery
The success of your surgery will depend in large measure on how well you follow our instructions regarding home care during the first few weeks after surgery.
Wound Care
You will have stitches or staples running along your wound or a suture beneath your skin. The stitches or staples will be removed approximately 2 weeks after surgery.
Avoid getting the wound wet until it has thoroughly sealed and dried. A bandage may be placed over the wound to prevent irritation from clothing or support stockings.
Diet
Some loss of appetite is common for several weeks after surgery. A balanced diet, often with an iron supplement, is important to promote proper tissue healing and restore muscle strength. Be sure to drink plenty of fluids.
Activity
Exercise is a critical component of home care, particularly during the first few weeks after surgery. You should be able to resume most normal light activities of daily living within 3 to 6 weeks following surgery. Some discomfort with activity and at night is common for several weeks.
Your activity program should include:
- A graduated walking program, initially in your home and later outside
- A walking program to slowly increase your mobility and endurance
- Resuming other normal household activities
- Resuming sitting, standing, and walking up and down stairs
- Specific exercises several times a day to restore movement
-
Specific exercises several times a day to strengthen your hip joint
- You may wish to have a physical therapist help you at home
Avoiding Problems After Surgery
Blood Clot Prevention
Follow our instructions carefully to minimize the potential risk of blood clots, which can occur during the first several weeks of your recovery.
Warning Signs
Warning signs of possible blood clots include:
- Pain in your calf and leg that is unrelated to your incision
- Tenderness or redness of your calf
- Swelling of your thigh, calf, ankle, or foot
Warning signs that a blood clot has traveled to your lung include:
- Shortness of breath
- Chest pain, particularly with breathing
Notify us immediately if you develop any of these signs.
Preventing Infection
The most common causes of infection following hip replacement surgery are from bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your prosthesis.
Following your surgery, you may need to take antibiotics prior to dental work, including dental cleanings, or any surgical procedure that could allow bacteria to enter your bloodstream.
Warning signs of a possible hip replacement infection are:
- Persistent fever (higher than 100°F orally)
- Shaking chills
- Increasing redness, tenderness, or swelling of the hip wound
- Drainage from the hip wound
- Increasing hip pain with both activity and rest
Avoiding Falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery. Stairs are a particular hazard until your hip is strong and mobile. You should use a cane, crutches, a walker, or handrails or have someone help you until you improve your balance, flexibility, and strength.
Your physical therapist will help you decide which assistive aides will be required following surgery, and when those aides can safely be discontinued.
Other Precautions
To assure proper recovery and prevent dislocation of the prosthesis, you must take special precautions:
- Do not cross your legs.
- Do not bend your hips more than a right angle (90°).
- Do not turn your feet excessively inward or outward.
- Use a pillow between your legs at night when sleeping until you are advised by us that you can remove it.
We will give you more instructions prior to your discharge from the hospital.
How Your New Hip Is Different
You may feel some numbness in the skin around your incision. You also may feel some stiffness, particularly with excessive bending. These differences often diminish with time, and most patients find these are minor compared with the pain and limited function they experienced prior to surgery.
Your new hip may activate metal detectors required for security in airports and some buildings. Tell the security agent about your hip replacement if the alarm is activated. You may ask us for a card confirming that you have an artificial hip.
After surgery, make sure you also do the following:
- Participate in a regular light exercise program to maintain proper strength and mobility of your new hip.
- Take special precautions to avoid falls and injuries. Individuals who have undergone hip replacement surgery and experience a fracture may require more surgery.
- Notify your dentist that you have had a hip replacement. You will need to take antibiotics before any dental procedure for a minimum of 2 years after your surgery and possibly longer, depending on your past health history.
- You need to be seen periodically for routine follow-up examinations and x-rays (radiographs), even if your hip replacement seems to be doing fine.
