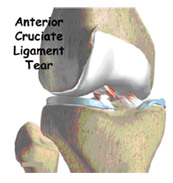
ACL Injury: Does It Require Surgery?

The anterior cruciate ligament (ACL) is one of the most commonly injured ligaments of the knee. The incidence of knee ligament injuries in the general population. In general, the incidence of ACL injury is higher in people who participate in high-risk sports, such as basketball, football, skiing, and soccer. However,ACL injuries are very commonly seen with road traffic accidents also.
As sports have become an increasingly important part of day-to-day life over the past few decades, the number of ACL injuries has steadily increased. This injury has received a great deal of attention from orthopedic surgeons over the past 15 years, and is one of the most successful surgeries in the field of Arthroscopic surgery today.
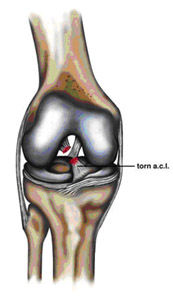
Anatomy and Pathophysiology
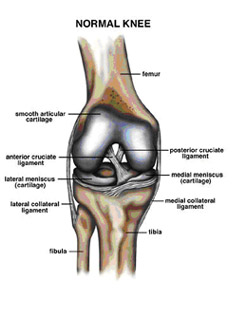
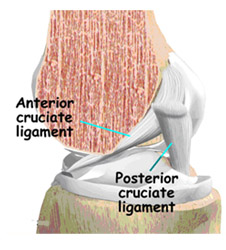
The bone structure of the knee joint is formed by the femur, the tibia, and the patella. The ACL is one of the four main ligaments within the knee that connect the femur to the tibia.
The knee is essentially a hinged joint that is held together by the medial collateral (MCL), lateral collateral (LCL), anterior cruciate (ACL) and posterior cruciate (PCL) ligaments. The ACL runs diagonally in the middle of the knee, preventing the tibia from sliding out in front of the femur as well as providing rotational stability to the knee.
The weight-bearing surface of the knee is covered by a layer of articular cartilage. On either side of the joint, between the cartilage surfaces of the femur and tibia, are the medial meniscus and lateral meniscus. The menisci act as shock absorbers and work with the cartilage to reduce the stresses between the tibia and the femur.
Mechanism of injury

It is estimated that 70 percent of ACL injuries occur through non-contact mechanisms while 30 percent result from direct contact with another player or object.The mechanism of injury is often associated with deceleration coupled with cutting, pivoting or sidestepping maneuvers, awkward landings or "out of control" play.Female athletes have a higher incidence of ACL injury than male athletes in certain sports This is due to differences in physical conditioning, muscular strength, and neuromuscular control.
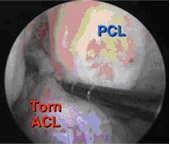
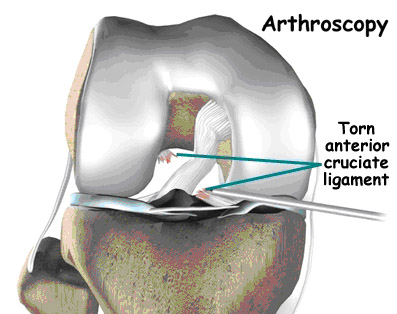
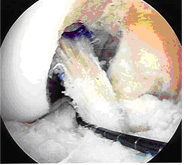
Arthroscopic picture of torn ACL
Approximately 50 percent of ACL injuries occur in combination with damage to the meniscus, articular cartilage, or other ligaments. Additionally, patients may have bone bruises of the bone beneath the cartilage surface. These may be seen on an MRI and may indicate injury to the overlying articular cartilage.
Symptoms
Immediately after the injury, patients usually experience pain and swelling and the knee feels unstable. Within a few hours after a new ACL injury, patients often have a large amount of knee swelling, a loss of full range of motion, pain or tenderness along the joint line and discomfort while walking.
The instability caused by the torn ligament leads to a feeling of insecurity and giving way of the knee, especially when trying to change direction on the knee. The knee may feel like it wants to slip backwards.
The pain and swelling from the initial injury will usually be gone after two to four weeks, but the knee may still feel unstable. The symptom of instability and the inability to trust the knee for support are what require treatment. Also important in the decision about treatment is the growing realization that long-term instability leads to early arthritis of the knee.
Diagnosis
The history and physical examination are probably the most important ways to diagnose a ruptured or deficient ACL. In the acute (sudden) injury, the swelling is a good indicator. A good rule of thumb that is used is that any tense swelling that occurs within two hours of a knee injury usually represents blood in the joint, or a hemarthrosis. If the swelling occurs the next day, the fluid is probably from the inflammatory response.
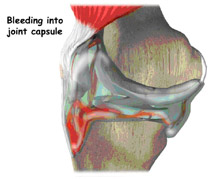
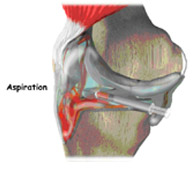
Placing a needle in the swollen joint and aspirating gives relief from the swelling and provides useful information . If blood is found when draining the knee, there is about a 70 percent chance it represents a torn ACL. This fluid can also show if the cartilage on the surface of the knee joint was injured.
During the physical examination , we will determine how badly the ACL was injured and whether other knee ligaments or joint cartilage were injured. If the ACL is torn, there will be increased forward (upward or anterior) movement of the tibia in relation to the femur (especially when compared to the normal leg) and a soft, mushy endpoint when this movement ends ( Lachman’s test ). The second test is the Lachman's Test video pivot shift test . Pivot Shift Test vide. In this test, if the ACL is torn, the tibia will start forward when the knee is fully straight and then will shift back into the correct position in relation to the femur when the knee is bent past 30 degrees.
X-rays of the knee are done to rule out a fracture. Ligaments and tendons do not show up on X-rays, but bleeding into the joint can result from a fracture of the knee joint . MRI Scan is probably the most accurate test for diagnosing a torn ACL without actually looking into the knee. This test does not require any needles or special dye and is painless.
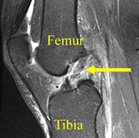
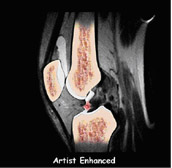
MRI of complete ACL tear
In some cases, arthroscopy may be used to make the definitive diagnosis if there is a question about what is causing your knee problem.
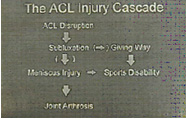
Natural History
The natural history of an ACL injury without surgical intervention varies from patient to patient and depends on the patient's activity level, degree of injury and instability symptoms.
The prognosis for a partially torn ACL without instability symptoms is sometimes favorable, with the recovery and rehabilitation period usually at least 3 months. However close clinical follow-up and a complete course of physical therapy should be done to identify those patients with unstable knees due to partial ACL tears.
Complete ACL ruptures have a much less favorable outcome. After a complete ACL tear, some patients are unable to participate in cutting or pivoting-type sports, while others have instability during even normal activities such as walking. There are some rare individuals who can participate in sports without any symptoms of instability. This variability is related to the severity of the original knee injury as well as the physical demands of the patient.
About half of ACL injuries occur in combination with damage to the meniscus, articular cartilage or other ligaments. Secondary damage may occur in patients who have repeated episodes of instability due to ACL injury. With chronic instability, up to 90 percent of patients will have meniscus damage when reassessed 10 or more years after the initial injury. Similarly, the prevalence of articular cartilage lesions increases up to 70 percent in patients who have a 10-year-old ACL deficiency.
Arthroscopic picture of damaged articular cartilage in chronically ACL-deficient knee.
Surgical and Non-Surgical Options
Treatment options for ACL injuries include both surgical and non surgical treatments.
Nonsurgical Treatment Benefits and Limits
Surgical treatment is usually advised in dealing with combined injuries (ACL tears in combination with other injuries in the knee). However, deciding against surgery is reasonable for select patients. Non surgical management of isolated ACL tears is likely to be successful or may be indicated in patients:
- With partial tears and NO instability symptoms.
- With complete tears and no symptoms of knee instability during low-demand sports who are willing to give up high-demand sports
- Who do light manual work or live sedentary lifestyles
- Whose growth plates are still open (children)
In non surgical treatment, progressive physical therapy and rehabilitation can restore the knee to a condition close to its pre-injury state and educate the patient on how to prevent instability.This may be supplemented with the use of a hinged knee brace. However, many people who choose not to have surgery may experience secondary injury to the knee due to repetitive instability episodes.
So in summary , a patient who opts for non surgical treatment has to remember :
- Modification of active lifestyle to avoid high demand activities
- Muscle strengthening exercises for life
- May require knee brace
- Despite above precautions ,secondary damage to knee cartilage & meniscus leading to premature arthritis .
Surgical Intervention and Considerations
ACL tears are not usually repaired using suture to sew it back together, because repaired ACLs have generally been shown to fail over time.Therefore, the torn ACL is generally replaced by a substitute graft made of tendon. The grafts commonly used to replace the ACL include:
- Patellar tendon autograft (autograft comes from the patient)
- Hamstring tendon autograft
- Quadriceps tendon autograft
- Allograft (taken from a cadaver) patellar tendon, Achilles tendon, semitendinosus, gracilis, or posterior tibialis tendon
Patients treated with surgical reconstruction of the ACL have long-term success rates of over 95 percent. Recurrent instability and graft failure are seen in approximately 1-2 percent of patients. The goal of the ACL reconstruction surgery is to prevent instability and restore the function of the torn ligament, creating a stable knee. This allows the patient to return to sports. There are certain factors that the patient must consider when deciding for or against ACL surgery.
Patient Considerations
Active adult patients involved in sports or jobs that require pivoting, turning or hard-cutting as well as heavy manual work are encouraged to consider surgical treatment.This even includes older patients . Activity, not age, should determine if surgical intervention should be considered.
In young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems. We can delay ACL surgery until the child is closer to skeletal maturity but it is better to operate & modify the ACL surgery technique to decrease the risk of growth plate injury .
A patient with a torn ACL and significant functional instability has a high risk of developing secondary knee damage and should therefore consider ACL reconstruction.
It is common to see ACL injuries combined with damage to the menisci (50 percent), articular cartilage (30 percent), collateral ligaments (30 percent), joint capsule, or a combination of the above. The "unhappy triad", frequently seen in football players and skiers, consists of injuries to the ACL, the MCL and the medial meniscus. In cases of combined injuries, surgical treatment may be warranted and generally produces better outcomes.
Surgical Choices
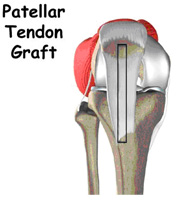

The middle third of the patellar tendon of the patient, along with a bone plug from the shin and the knee cap is used in thepatellar tendon autograft. Occasionally referred to by some surgeons as the "gold standard" for ACL reconstruction, it is often recommended for high-demand athletes and patients whose jobs do not require a significant amount of kneeling. However, patellar tendon autografts have a small risk of postoperative patellofemoral pain (pain behind the kneecap) complaints and other problems if the postoperative rehabilitation is not followed appropriately.
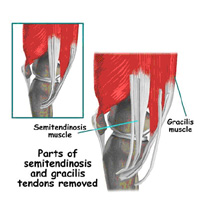
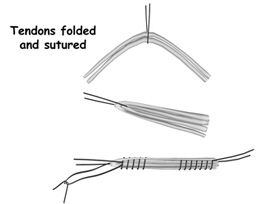
The semitendinosus & gracilis hamstring tendons on the inner side of the knee are used in creating thehamstring tendon autograft for ACL Reconstruction. This creates a four-strand tendon graft. Hamstring graft proponents claim there are fewer problems associated with harvesting of the graft compared to the patellar tendon autograft including:
- Fewer problems with anterior knee pain or kneecap pain after surgery
- Less postoperative stiffness problems
- Faster recovery
The graft function may be limited by the strength and type of fixation in the bone tunnels, as the graft does not have bone plugs. There have been conflicting results in research studies as to whether hamstring grafts are slightly more susceptible to graft elongation (stretching), which may lead to increased laxity during objective testing. The quadriceps tendon autograft is often used for patients who have already failed ACL reconstruction. The middle third of the patient's quadriceps tendon and a bone plug from the upper end of the knee cap are used . Patients may find the incision not cosmetically appealing.
Allografts are grafts taken from cadavers and are becoming increasingly popular.These grafts are also used for patients who have failed ACL reconstruction before and in surgery to repair or reconstruct more than one knee ligament. Advantages of using allograft tissue include elimination of obtaining the graft from the patient, decreased surgery time and smaller incisions.
However, allografts are associated with a risk of infection, including viral transmission (HIV and Hepatitis C), despite careful screening and processing . There have also been conflicting results in research studies as to whether allografts are slightly more susceptible to graft elongation (stretching), which may lead to increased laxity during testing.
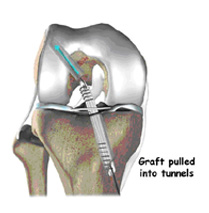
Surgical Procedure ( Arthroscopic ACL Reconstruction)
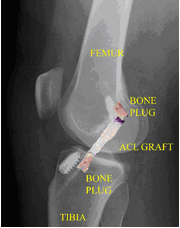
Post-operative X-ray after ACL patellar tendon reconstruction
The patient, the surgeon and the anesthethist select the anesthesia used for surgery. We usually prefer Regional anaesthesia as it provides postoperative pain control and also allows the patient to visualise the procedure on the monitor . The surgery usually begins with an examination of the patient's knee while the patient is relaxed due the effects of anesthesia. This final examination is used to verify that the ACL is torn and also to check for looseness of other knee ligaments that may need to be repaired during surgery or addressed postoperatively . If the physical exam strongly suggests the ACL is torn, the selected graft is harvested and prepared to the correct size for the patient.
After the graft has been prepared, we place an arthroscope into the joint. Small 5mm incisions called portals are made in the front of the knee to insert the arthroscope and instruments and we examine the condition of the knee.
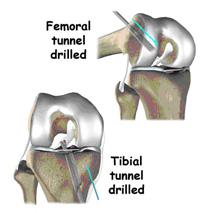
Meniscus and cartilage injuries are trimmed or repaired and the torn ACL stump is then removed. In the most common ACL reconstruction technique, bone tunnels are drilled into the tibia and the femur to place the ACL graft in almost the same position as the torn ACL. A long needle is then passed through the tunnel of the tibia, up through the femoral tunnel, and then out through the skin of the thigh. The sutures of the graft are placed through the eye of the needle and the graft is pulled into position up through the tibial tunnel and then up into the femoral tunnel. The graft is held under tension as it is fixed in place using interference screws, spiked washers, posts or staples. The devices used to hold the graft in place are generally not removed.
Before the surgery is complete, we will probe the graft to make sure it has good tension, verify that the knee has full range of motion and perform tests such as the Lachman's test to assess graft stability. The skin is closed and dressings along with a hinged knee brace are applied. The patient will usually go home the next day after surgery.
Potential Surgical Complications
The incidence of infection after arthroscopic ACL reconstruction has a reported range of 0.2 percent to 0.48 percent . It is lower than open surgery because of the constant irrigation of the joint with the distending fluid .
Allografts specifically are associated with risk of viral transmission, including HIV and Hepatitis C, despite careful screening and processing .
Rare risks include bleeding , nerve injury & blood clots . It is not uncommon to have numbness of the outer part of the upper leg next to the incision, which is temporary.
Recurrent instability due to rupture or stretching of the reconstructed ligament or poor surgical technique (reported to be as low as 2.5 percent and as high as 10 percent) is possible.
Other rare complications reported are knee stiffness & patellar fractures .
In young children or adolescents with ACL tears, early ACL reconstruction creates a possible risk of growth plate injury, leading to bone growth problems. This can be circumvented by modification of the surgical procedure as the risk of delaying surgery in an active boy may be higher.
Postoperative anterior knee pain is sometimes seen patellar tendon autograft ACL reconstruction especially if the postoperative rehabilitation programme is not followed aggressively .
Rehabilitation/Convalescence
Postoperative Course
Physical therapy is a crucial part of successful ACL surgery, with exercises beginning immediately after the surgery. Much of the success of ACL reconstructive surgery depends on the patient's dedication to rigorous physical therapy. With new surgical techniques and stronger graft fixation, current physical therapy uses an accelerated course of rehabilitation .
In the first 10 to 14 days after surgery, the wound is kept clean and dry, and early emphasis is placed on regaining the ability to fully straighten the knee and restore quadriceps control. The knee is iced regularly to reduce swelling and pain. We use a postoperative brace Weight bearing status (use of crutches to keep some or all of the patient's weight off of the surgical leg) is also determined by physician preference, as well as other injuries addressed at the time of surgery.
Rehabilitation


The goals for rehabilitation of ACL reconstruction include reducing knee swelling, maintaining mobility of the kneecap to prevent anterior knee pain problems, regaining full range of motion of the knee, as well as strengthening the quadriceps and hamstring muscles.
As the rehabilitation program evolves, more challenging exercises are chosen to safely advance the knee's strength and function. Specialized balance exercises are used to help the muscles respond quickly and without thinking. This part of treatment is called neuromuscular training. If you need to stop suddenly, your muscles must react with just the right amount of speed, control, and direction. After ACL surgery, this ability doesn't come back completely without exercise.
Neuromuscular training includes exercises to improve balance, joint control, muscle strength and power, and agility. Agility makes it possible to change directions quickly, go faster or slower, and improve starting and stopping. These are important skills for walking, running, and jumping, and especially for sports performance.
The patient may return to sports when there is no longer pain or swelling, when full knee range of motion has been achieved, and when muscle strength, endurance and functional use of the leg have been fully restored . This usually takes 4 to 6 months. The use of a functional brace when returning to sports is ideally not needed after a successful ACL reconstruction, but some patients may feel a greater sense of security by wearing one. Ideally you are able to resume all your previous lifestyle activities including participating in sports .
SUMMARY
ACL injuries are on the rise and are a cause for serious disability to people keen to pursue sporting activities . There is also a high risk of premature arthritis of the knee in patients not opting for surgical management
Arthroscopic ACL reconstruction is one of the most successful surgeries in orthopaedic surgery . It involves a 1 inch incision to harvest the graft and takes about 45 min to perform the procedure . The decision on which graft to use and what type of fixation varies from person to person and is best decided by your surgeon.
The postoperative physical therapy programme is very important for an optimum outcome and includes neuromuscular training along with regular exercises .
As outcome of the procedure depends on the surgical expertise of the surgeon , you should choose your surgeon based on his experience in this field to minimise the risk of complications .
