Dislocating shoulder ( shoulder instability )
Introduction
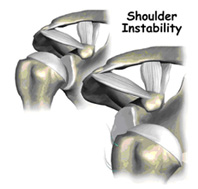
Shoulder instability means that the shoulder joint is too loose and is able to slide around too much in the socket. In some cases, the unstable shoulder actually slips out of the socket. If the shoulder slips completely out of the socket, it has become dislocated. If not treated, instability can lead to arthritis of the shoulder joint.
What parts of the shoulder are involved?
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone,) and the clavicle (collarbone).
The rotator cuff connects the humerus to the scapula. The rotator cuff is actually made up of the tendons of four muscles: the supraspinatus, infraspinatus, teres minor, and subscapularis.
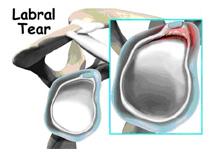
Tendons attach muscles to bones. Muscles move bones by pulling on tendons. The muscles of the rotator cuff also keep the humerus tightly in the socket. A part of the scapula, called the glenoid, makes up the socket of the shoulder. The glenoid is very shallow and flat. A rim of soft tissue, called the labrum, surrounds the edge of the glenoid, making the socket more like a cup. The labrum turns the flat surface of the glenoid into a deeper socket that molds to fit the head of the humerus.
Surrounding the shoulder joint is a watertight sac called the joint capsule. The joint capsule holds fluids that lubricate the joint. The walls of the joint capsule are made up of ligaments. Ligaments are soft connective tissues that attach bones to bones. The joint capsule has a considerable amount of slack, loose tissue, so that the shoulder is unrestricted as it moves through its large range of motion. If the shoulder moves too far, the ligaments become tight and stop any further motion, sort of like a dog coming to the end of its leash.
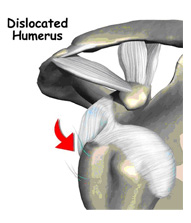
Dislocations happen when a force overcomes the strength of the rotator cuff muscles and the ligaments of the shoulder. Nearly all dislocations are anterior dislocations, meaning that the humerus slips out of the front of the glenoid. Only three percent of dislocations are posterior dislocations, or out the back.
Sometimes the shoulder does not come completely out of the socket. It slips only partially out and then returns to its normal position. This is called subluxation
What makes a shoulder unstable?
Shoulder instability often follows an injury that caused the shoulder to dislocate. This initial injury is usually fairly significant, and the shoulder must be reduced. To reduce a shoulder means it must be manually put back into the socket. The shoulder may seem to return to normal, but the joint often remains unstable. The ligaments that hold the shoulder in the socket, along with the labrum (the cartilage rim around the glenoid), may have become stretched or torn. This makes them too loose to keep the shoulder in the socket when it moves in certain positions. An unstable shoulder can result in repeated episodes of dislocation, even during normal activities. Instability can also follow less severe shoulder injuries.
In some cases, shoulder instability can happen without a previous dislocation. People who do repeated shoulder motions may gradually stretch out the joint capsule. This is especially common in athletes such as baseball pitchers, volleyball players, and swimmers. If the joint capsule gets stretched out and the shoulder muscles become weak, the ball of the humerus begins to slip around too much within the shoulder. Eventually this can cause irritation and pain in the shoulder.
A genetic problem with the connective tissues of the body can lead to ligaments that are too elastic. When ligaments stretch too easily, they may not be able to hold the joints in place. All the joints of the body may be too loose. Some joints, such as the shoulder, may be easily dislocated. People with this condition are sometimes referred to as double-jointed.
What problems does an unstable shoulder cause?
Chronic instability causes several symptoms. Frequent subluxation is one. In subluxation, the shoulder may slip (sublux) in certain positions, and the shoulder may actually feel loose. This commonly happens when the hand is raised above the head, for example while throwing. Subluxation of the shoulder usually causes a quick feeling of pain, like something is slipping or pinching in the shoulder. Over time, you may stop using the shoulder in ways that cause subluxation.
The shoulder may become so loose that it starts to dislocate frequently. This can be a real problem, especially if you can't get it back in the socket and must go to the emergency room every time. A shoulder dislocation is usually very obvious. The injury is very painful, and the shoulder looks abnormal. Any attempted shoulder movements cause extreme pain. A dislocated shoulder can damage the nerves around the shoulder joint.
Once a labral tear develops , symptoms include
- Pain, usually with overhead activities
- Catching, locking, popping, or grinding
- Occasional night pain or pain with daily activities
- A sense of instability in the shoulder
- Decreased range of motion
- Loss of strength
Diagnosis
The diagnosis of shoulder instability is primarily done through your medical history and physical exam. The medical history will include many questions about past shoulder injuries, your pain, and the ways your symptoms are affecting your activities.
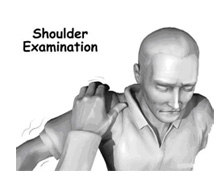
In the physical exam, we will feel and move your shoulder, checking it for strength and mobility. We will stress the shoulder to test the ligaments. When the shoulder is stretched in certain directions, you may get the feeling that the shoulder is going to dislocate. This is a very important sign of instability. It is called an apprehension sign. (Don't worry. Unless your shoulder is extremely loose, it will not dislocate.)
You will have an X-ray. X-rays can help confirm that your shoulder was dislocated or injured in the past.
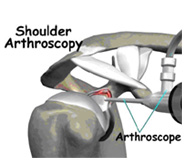
If your diagnosis is unsure , an MRI Scan is helpful. Finally an examination under anaesthesia ( EUA ) is done followed by a shoulder arthroscopy . An arthroscope is a tiny TV camera inserted into the shoulder through a small incision. This allows a good look at the muscles and ligaments of the shoulder. When you are awake, it is hard to test the ligaments because you automatically tighten the muscles during the exam.
When you come with an acutely dislocated shoulder, X-rays are necessary to rule out a fracture. X-rays are usually done after the shoulder is put back into joint. This allows us to make sure the joint is back in place.
What treatment options are available?
Non surgical treatment
The first goal will be to help you control your pain and inflammation. Initial treatment to control pain is usually rest and anti-inflammatory medication . You may need a cortisone injection if you have trouble getting your pain under control. Cortisone is a strong anti-inflammatory medication.
The physical therapist will direct your rehabilitation program. At first, patients are shown ways to avoid positions and activities that put the shoulder at further risk of injury or dislocation. Overhand athletes may be issued a special shoulder strap or sleeve to stop the shoulder from moving in ways that strain it.
The therapist may use heat or ice treatments to ease pain and inflammation. Hands-on treatments and various types of exercises are used to improve the range of motion in your shoulder and nearby joints and muscles. Later, you will do strengthening exercises to improve the strength and control of the rotator cuff and shoulder blade muscles. Your therapist will help you retrain these muscles to keep the ball of the humerus in the socket. This will improve the stability of the shoulder and help your shoulder joint move smoothly.
You may need therapy treatments for six to eight weeks. Most patients are able to get back to their activities with full use of their arm within this amount of time.
Surgery
If your therapy program doesn't stabilize your shoulder after a period of time, you may need surgery. There are many different types of shoulder operations to stabilize the shoulder. Almost all of these operations attempt to tighten the ligaments that are loose. The loose ligaments are usually along the front or bottom part of the shoulder capsule.
Bankart Repair
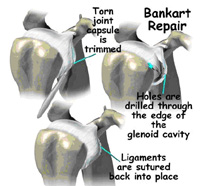
The most common method for surgically stabilizing a shoulder that is prone to anterior dislocations is the Bankart repair. The Bankart repair involves sewing or stapling ligaments, along with the labrum, on the front side of the joint back into their original position.
In a Bankart repair, we first clear away any frayed or torn edges. Holes for the sutures are drilled into the scapula bone. The capsular ligaments and labrum are then attached with sutures to the bone. The ligaments heal, and scar tissue eventually anchors the ends to the bone. With the ligaments back in place, the joint is much more stable.
Typically the Bankart repair is done through an incision on the front of the shoulder. We are doing it Arthroscopically in selected cases . Arthroscopes require smaller incisions, which means less time in the hospital and less time to heal.
Capsular Shift
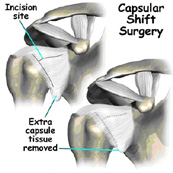
Another surgery to tighten a loose shoulder joint is a procedure called a capsular shift. In this procedure, an incision is made on the front of the joint capsule to create a flap. The flap of tissue is pulled over the front of the capsule and sewn together. This is similar to when a tailor tucks loose fabric by overlapping and sewing the two parts together.
Thermal Capsular Shrinkage
There is a newer procedure called thermal capsular shrinkage. Using an arthroscope, we slides an electrode probe inside the unstable shoulder. The electrode is heated up, and we move the probe over the injured ligament. The heat causes the capsule to shrink and tighten. One of the risks with this type of surgery is that the capsule may get too tight, leading to restricted shoulder motion.
Rehabilitation
Non-surgical rehabilitation
The goal of therapy will be to strengthen the rotator cuff and shoulder blade muscles to make the shoulder more stable. At first you will do exercises with a therapist. Eventually you will be put on a home program of exercise to keep the muscles strong and flexible. This should help you avoid future problems.
After Surgery
Rehabilitation after surgery is more complex. You will likely wear a sling to support and protect the shoulder for one to four weeks. A physical or occupational therapist may direct your recovery program. Depending on the surgical procedure, you will probably need to attend therapy sessions for two to four months. You should expect full recovery to take up to six months.
The first few therapy treatments will focus on controlling the pain and swelling from surgery. Ice and electrical stimulation treatments may help. Your therapist may also use massage and other types of hands-on treatments to ease muscle spasm and pain.
Therapy after Bankart surgery proceeds slowly. Range-of-motion exercises begin soon after surgery, but therapists are cautious about doing stretches on the front part of the capsule for the first six to eight weeks. The program gradually works into active stretching and strengthening.
Therapy goes even slower after surgeries where the front shoulder muscles have been cut. Exercises begin with passive movements. During passive exercises, your shoulder joint is moved, but your muscles stay relaxed. Your therapist gently moves your joint and gradually stretches your arm. You may be taught how to do passive exercises at home.
Active therapy starts three to four weeks after surgery. You use your own muscle power in active range-of-motion exercises. You may begin with light isometric strengthening exercises. These exercises work the muscles without straining the healing tissues.
At about six weeks you start doing more active strengthening. Exercises focus on improving the strength and control of the rotator cuff muscles and the muscles around the shoulder blade. Your therapist will help you retrain these muscles to keep the ball of the humerus in the socket. This helps your shoulder move smoothly during all your activities.
By about the tenth week, you will start more active strengthening. These exercises focus on improving strength and control of the rotator cuff muscles. Strong rotator cuff muscles help hold the ball of the humerus tightly in the glenoid to improve shoulder stability.
Overhand athletes (such as those who throw baseballs or footballs) start gradually in their sport activity about three months after surgery. They can usually return to competition within four to six months.
Some of the exercises you'll do are designed to get your shoulder working in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don't put too much stress on your shoulder. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
